
About Mo
M o Kasti is a distinguished author, thinker, speaker, strategy advisor and family man. His passion is to inspire others to lead with heart, purpose and courage, think uncommonly, and harness of the power of “Us” to deliver innovative and exceptional outcomes.
Mo works with leaders, teams and organizations on leadership, strategy, innovation, and organizational/cultural transformation. When terrains are shifting, and outcomes are uncertain, Mo is uniquely equipped to help leaders think outside the box. He is sought after for his expertise in strategy, innovation, growth, and organizational renewal.
Mo is part of MG100 Global Coaches and has received the award from Marshall Goldsmith as the #1 MG Healthcare Leadership Coach. He is also the author of two Healthcare Leadership books: Physician Leadership: The Rx for Healthcare Transformation and Beyond Physician Engagement- How to have your team be ALL IN.
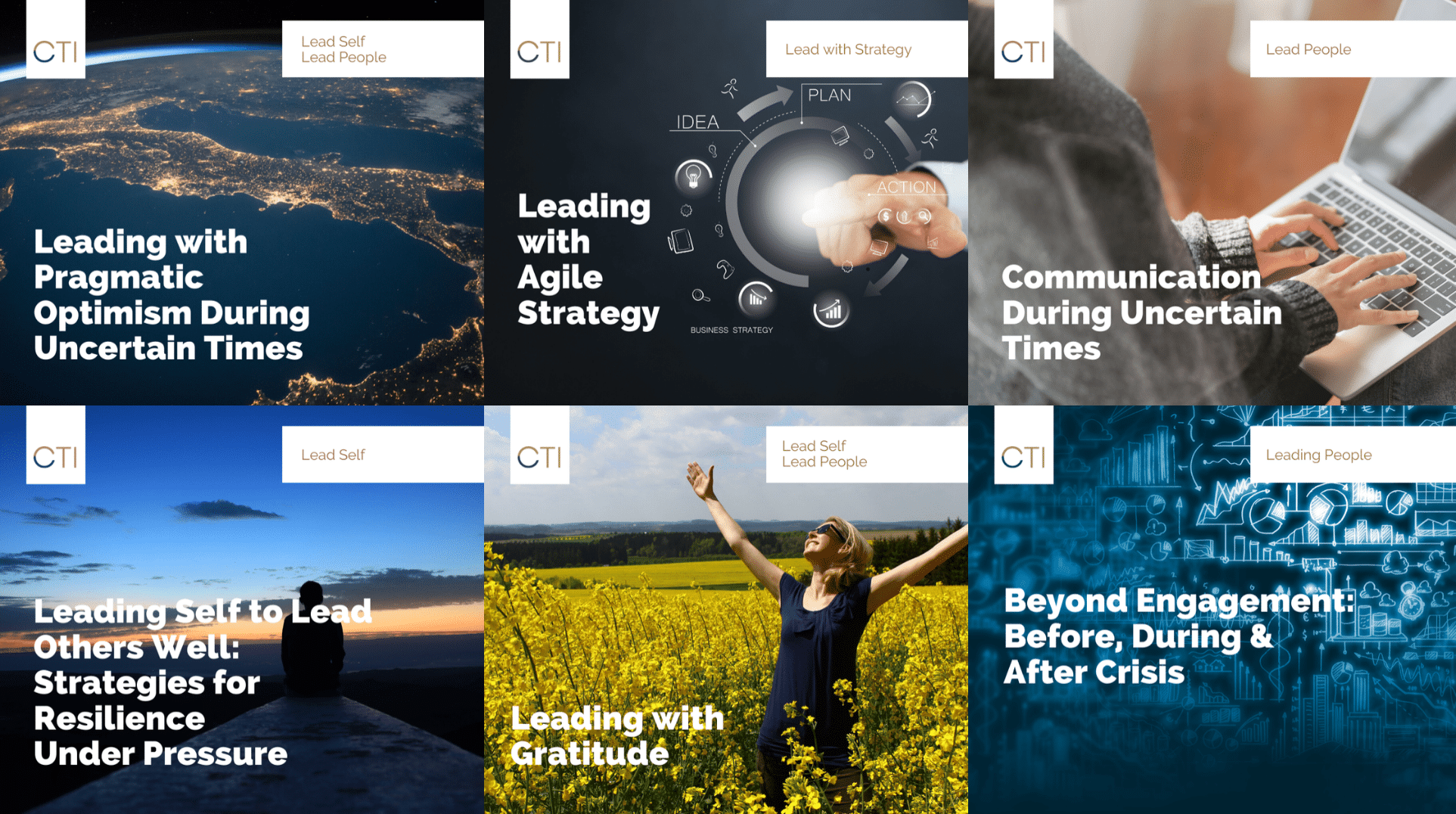
Virtual Webinars
Mo’s webinars focus on an array of leadership, strategy and innovation topics and are specifically designed to meet your development needs in a timely and convenient way. They are built around his five Disciplines of Transformational Leadership and directly align with the structure of with CTI's leadership development curriculum: Leading Self, Leading People, Leading with Strategy, Leading for Results, Leading with Purpose.

Beyond Physician Engagement
As CEO of CTI’s Physician Leadership Institute, Mo has seen the power of strong physician engagement firsthand. His book reveals real-life examples of leaders who have been successful at engaging their physicians by acting as partners: co-leading, co-creating, and working together to establish trust. It provides readers with a progressive roadmap that blends the art of leadership, neuroscience, language, and conversation.
Mo's Blog Articles
July 11, 2016
In June, we lost an American icon and dearly beloved sports hero with the passing of Muhammad Ali. Ali will forever be known as “the greatest” […]
